Preventing endometriosis recurrence: expert-led, evidence-based care
Endometriosis affects nearly one in ten women of reproductive age worldwide, making it one of the most common and challenging gynecological conditions today. Even after treatment, many women remain anxious about symptoms returning, pain resurfacing, or fertility being affected. Preventing endometriosis recurrence is therefore not just about symptom relief, but about long-term, well-planned medical care that is rooted in science and clinical experience.
This comprehensive approach is offered by Dr Meera B, a senior gynecologist with more than thirty years of experience in women’s health and reproductive medicine. Consulting at leading hospitals including Aster PMF Hospital, Sasthamkotta, Dr Meera B provides ethical, evidence-based guidance that prioritizes patient safety, long-term outcomes, and informed decision-making.
How to prevent endometriosis from recurring?
The most reliable way to address how to prevent endometriosis from recurring is through a structured, individualized care plan. Endometriosis is a chronic condition influenced by hormones, immune responses, and anatomical factors. Because of this complexity, no single treatment works for everyone.
Dr Meera B emphasizes that recurrence prevention begins immediately after diagnosis or treatment. This may include careful post-surgical planning, appropriate hormonal management when indicated, and regular monitoring. Importantly, the goal is not aggressive or unnecessary intervention, but balanced care that reduces disease activity while preserving overall health and fertility.
Why does endometriosis come back in some women?
Understanding how to prevent endometriosis from coming back starts with understanding why recurrence happens. Even after successful surgery or medical therapy, microscopic disease may persist. Ongoing estrogen stimulation and inflammation can also reactivate symptoms over time.
Other contributing factors may include:
- Discontinuation of follow-up care too early
- Incomplete suppression of disease activity when needed
- Delayed evaluation of returning symptoms
With long-term guidance, these risks can be identified early and addressed in a medically appropriate way.
How to reduce risk of endometriosis after treatment?
Patients often ask how to reduce risk of endometriosis once they have already been diagnosed or treated. The answer lies in ongoing disease awareness and consistent medical supervision rather than short-term fixes.
At Dr Meera B’s place of practice, risk reduction strategies may include:
- Regular clinical follow-ups based on symptom patterns
- Judicious use of hormonal therapy where scientifically supported
- Monitoring pelvic health through appropriate investigations
- Addressing associated gynecological conditions that may worsen symptoms
This measured approach helps reduce flare-ups and avoids unnecessary interventions.
How to prevent retrograde menstruation and its clinical relevance
Many women search for how to prevent retrograde menstruation, as it is commonly discussed in relation to endometriosis. While retrograde menstruation itself cannot be completely stopped, its role in disease progression can be managed.
Medical strategies focus on controlling menstrual flow and hormonal balance rather than attempting to eliminate a natural physiological process. Dr Meera B ensures that such strategies are only recommended when medically indicated and safe for the individual patient.
How to prevent endometriosis from returning while planning pregnancy
For women hoping to conceive, concerns about how to prevent endometriosis from returning are closely tied to fertility planning. Suppressing disease activity must be carefully balanced with reproductive goals.
With advanced training in reproductive medicine and IVF, Dr Meera B helps patients make informed decisions regarding:
- Timing of conception after treatment
- When medical therapy may be paused or continued
- Use of assisted reproductive techniques when appropriate
This integrated approach reduces anxiety and supports better reproductive outcomes without compromising safety.
How to prevent miscarriage with endometriosis?
Another critical concern for patients is how to prevent miscarriage with endometriosis. While endometriosis can be associated with higher pregnancy risks in some women, careful pre-pregnancy evaluation and close monitoring significantly improve outcomes.
Dr Meera B focuses on:
- Optimizing uterine and pelvic health before conception
- Managing inflammation prior to pregnancy
- Providing appropriate support during early pregnancy
Importantly, patients are given realistic expectations based on medical evidence, without false promises or guarantees.
Long-term care at Dr Meera B’s place of practice
Preventing endometriosis recurrence is a long-term process rather than a one-time treatment. At Dr Meera B’s place of practice, patients benefit from continuity of care, extensive clinical experience, and access to advanced medical facilities available at the hospitals where she consults.
Women often realize that delaying expert consultation or relying on incomplete information can lead to repeated flare-ups, avoidable discomfort, and emotional stress. Early, expert-led care helps preserve health, fertility, and quality of life.
About Dr Meera B
Dr Meera B is a senior gynecologist and reproductive medicine specialist based in Kollam, Kerala. She holds MBBS, DGO, DNB (Obstetrics & Gynaecology), MRCOG (UK), and FRCOG (UK) qualifications. She graduated from Government Medical College, Trivandrum, and completed her post-graduation at Government Medical College, Kottayam.
With over thirty years of experience, Dr Meera B has helped women from India and abroad manage complex gynecological conditions and fertility challenges. Her training at Bourn Hall Clinic, Cambridge, has strengthened her evidence-based approach to reproductive medicine and IVF. She currently consults at leading hospitals, including Aster PMF Hospital, Sasthamkotta.
Take the next step toward long-term relief
If you are concerned about recurrence, fertility, or long-term symptom control, timely expert guidance can make a meaningful difference. To book an appointment with Dr Meera B, you may fill and submit the form at https://drmeerab.com/contact/, or call +91 9447145101. You may also send a WhatsApp message using the interface on the website to request an appointment. Dr Meera’s team will schedule your consultation and keep you informed.
Frequently Asked Questions on Preventing Endometriosis Recurrence
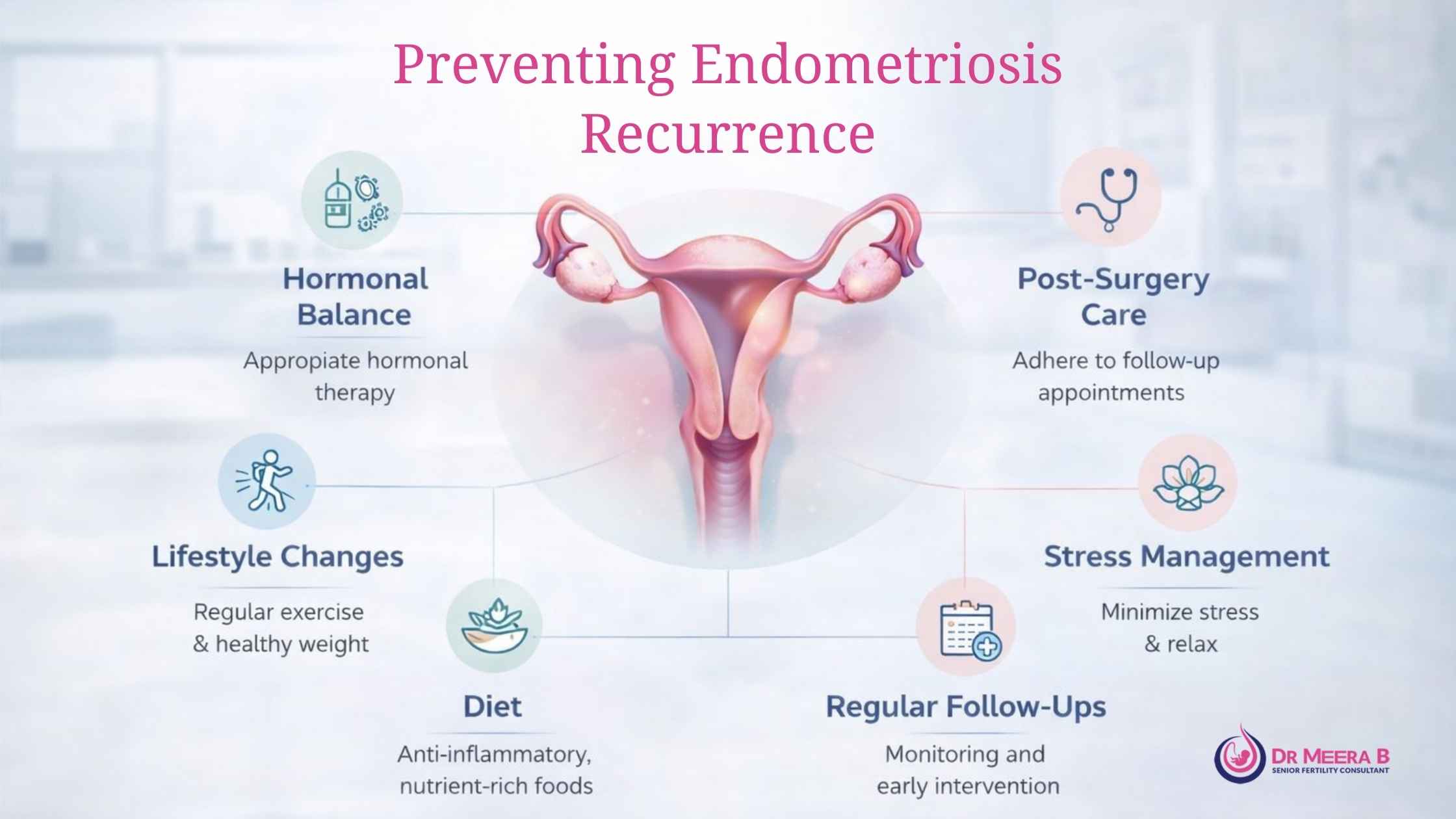
Preventing recurrence requires a long-term, individualized strategy that addresses hormonal balance, inflammation, and lifestyle factors. Patients often ask how to prevent endometriosis from recurring after surgery or medical treatment. Dr. Meera B emphasizes consistent follow-up care, appropriate hormonal therapy when indicated, anti-inflammatory nutrition, and stress management to reduce the chances of lesions reappearing and symptoms worsening over time.
Yes, recurrence refers to the regrowth or persistence of endometriotic lesions, while symptoms can return even without visible disease progression. Many women search for how to prevent endometriosis from coming back because pain or fatigue may reappear months or years later. Dr. Meera B evaluates both clinical symptoms and imaging findings to tailor preventive care that targets the root cause rather than symptoms alone.
Lifestyle choices play a meaningful role in disease control. Women seeking guidance on how to prevent endometriosis from returning are often advised to adopt an anti-inflammatory diet, maintain a healthy body weight, and prioritize restorative sleep. Under Dr. Meera B’s guidance, lifestyle measures are combined with medical management to support hormonal stability and long-term pelvic health.
Endometriosis can influence fertility by affecting egg quality, pelvic anatomy, and implantation. Many patients are concerned about how to prevent miscarriage with endometriosis, especially when planning pregnancy. Dr. Meera B focuses on optimizing uterine health, managing inflammation, and providing preconception care to improve pregnancy outcomes and reduce avoidable risks.
Medical strategies may include hormonal suppression, pain-modulating therapies, and close monitoring. Patients often ask how to reduce risk of endometriosis after treatment. Dr. Meera B carefully balances symptom relief with long-term health goals, ensuring therapies are adjusted over time rather than used as a one-size-fits-all solution.
Retrograde menstruation is one of the proposed mechanisms behind endometriosis development. Women frequently ask how to prevent retrograde menstruation as part of recurrence prevention. While it cannot be completely eliminated, Dr. Meera B may recommend cycle regulation and hormonal strategies to minimize its impact and reduce ongoing pelvic inflammation.

Comments are closed