Normal follicle size for pregnancy (By cycle day & mm)
Why follicle size matters when you are trying to conceive
A follicle is a fluid-filled sac in the ovary that contains an egg. Each cycle, multiple follicles begin to grow, but usually one becomes dominant. When that dominant follicle reaches the right size—and your hormones align—ovulation happens. Here’s the important part: the egg inside the follicle needs time to mature properly. That is why simply “seeing a follicle” isn’t enough. The relationship between follicle size, hormone readiness, and timing determines whether that month has a strong chance of success.What is the normal follicle size for pregnancy in mm?
In clinical practice, the “normal” size is the size at which the follicle is mature enough to release a mature egg and support fertilization. For most women, ovulation is expected when the dominant follicle is roughly:- 18–22 mm: most commonly associated with mature follicles and ovulation readiness
- 16–17 mm: may ovulate in some women, but egg maturity can vary
- 23–24 mm: can still ovulate, but may be slightly “post-mature” in some cases
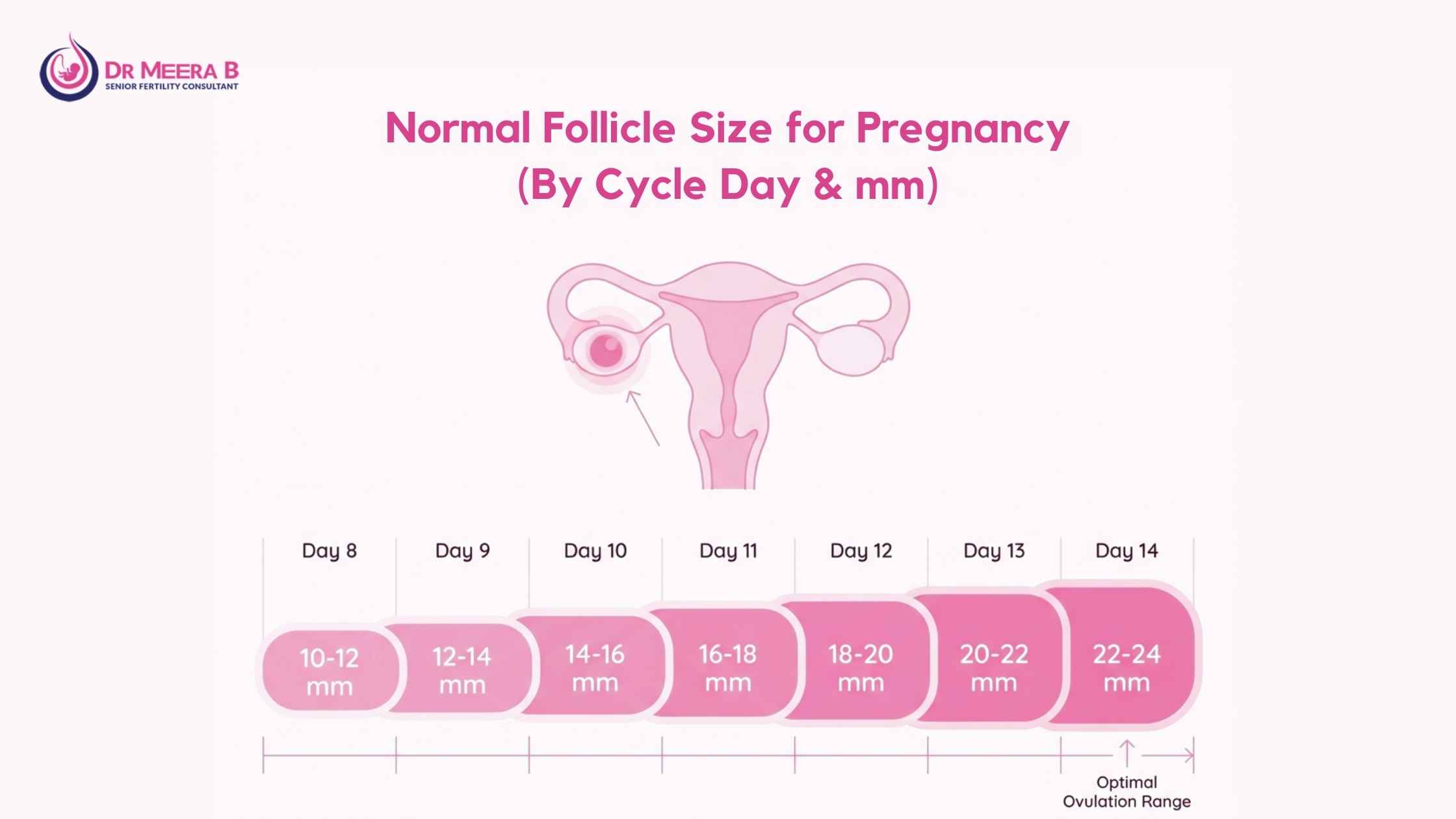
Follicle growth chart: What is expected by cycle day?
A typical dominant follicle grows about 1–2 mm per day after it becomes dominant (often around cycle day 7–9), and reaches around 18–22 mm near ovulation. Keep in mind that not every woman has a 28-day cycle, and ovulation does not always occur on day 14. That’s why ultrasound-based tracking is much more reliable than counting days.Typical follicular growth (example chart)
The following follicle growth chart represents an average 28–30 day cycle. Your personal numbers may vary (and that variation may still be completely normal).| Cycle day | What is happening in the ovary | Approx. dominant follicle size (mm) | What Dr Meera B typically looks for |
|---|---|---|---|
| Day 2–3 | Baseline scan; small follicles only | 2–6 mm | Good ovarian baseline; no cysts; AFC evaluation if needed |
| Day 7–9 | Selection of dominant follicle begins | 8–12 mm | Whether one follicle is “leading” appropriately |
| Day 10–12 | Rapid follicle growth | 13–17 mm | Endometrial thickness + follicle growth rate |
| Day 12–14 | Pre-ovulatory phase | 18–22 mm | Ovulation timing, trigger decision if needed |
| Day 14–16 | Ovulation likely occurs | Follicle collapses after rupture | Signs of rupture + free fluid; corpus luteum formation |
Ovulation ultrasound: What it shows (and what it does not)
An ovulation ultrasound is a transvaginal scan used to measure follicle size, monitor growth, assess uterine lining, and confirm if ovulation has happened. Patients often assume ultrasound only checks the ovary, but a fertility-focused scan evaluates multiple factors that affect pregnancy chances:- Dominant follicle size (the most obvious metric)
- Number of follicles developing
- Endometrial thickness and pattern (implantation readiness)
- Signs of ovulation (ruptured follicle, free fluid, corpus luteum)
Egg maturation: The missing link between size and actual fertility
Follicle size is a proxy for egg maturation, but it is not a guarantee. A follicle can be large without releasing a healthy mature egg, especially when hormonal imbalances or conditions like PCOS affect the cycle. This is one reason couples feel heartbroken after hearing “Your follicles look good” yet still not getting pregnant. The follicle might be the right size, but the egg may not be mature enough, or ovulation may not occur as expected.What supports healthy egg maturation?
- Accurate ovulation timing based on scan + symptoms
- Balanced hormones (thyroid, prolactin, insulin)
- Appropriate stimulation (when needed) under specialist supervision
- Healthy luteal phase support if medically indicated
What if the follicle is too small or too large?
When tracking, you may hear statements like “follicle is small” or “follicle is oversized.” Both can affect timing and outcomes, but neither is a reason to panic—especially if you are under expert guidance.If follicle size is too small
- Ovulation may occur late (common in longer cycles)
- Timing may be off if intercourse/IUI is planned too early
- May indicate hormonal imbalance, stress impact, or ovarian response concerns
If follicle size is too large
- It may ovulate later than expected
- Sometimes a follicle can become a functional cyst if it doesn’t rupture
- Egg quality may vary in post-mature follicles in certain contexts
Ideal follicle size IVF: What changes in fertility treatment?
The ideal follicle size IVF typically falls in the same maturity window—often around 18–22 mm—but IVF decisions are based on a cohort (group) of follicles, hormone levels, and planned egg retrieval timing. IVF is different from natural conception because the goal is not to release one egg; it’s to retrieve multiple mature eggs at the optimal time. That means follicle sizes can vary across the ovary, and decisions are personalized.In IVF, Dr Meera B focuses on “mature eggs”, not just big follicles
During stimulation cycles, follicles may grow in a range—some 14 mm, some 16 mm, and some in the prime 18–22 mm window. The fertility team chooses trigger timing to maximize maturity across the cohort.- Too early trigger: more immature eggs
- Too late trigger: risk of over-maturation and decreased quality in some eggs
- Right timing: better mature egg count and improved fertilization potential
When should you time intercourse or IUI based on follicle size?
In most cases, best timing is when the follicle measures around 18–22 mm and ovulation is expected within the next 24–48 hours, depending on hormonal signals and whether a trigger is used. General evidence-based timing guidelines:- Natural attempt: Intercourse on the day follicle is near 18 mm and the next 1–2 days
- Trigger cycle: Intercourse/IUI usually planned about 24–36 hours after trigger (as advised)
- If lining is thin: plan may include supporting endometrium before timing attempts
What results can you realistically expect with proper monitoring?
Fertility medicine is not about promising miracles. It is about improving odds with precision, discipline, and the right interventions at the right time. When follicle tracking and fertility evaluation are done properly, couples benefit from:- Clear identification of whether ovulation is truly happening
- More accurate fertile window timing
- Early detection of issues (PCOS patterns, luteal concerns, cysts)
- Faster movement to the right step—without wasting months
Why consult Dr Meera B for follicular tracking and fertility planning in Kerala?
Dr Meera B is a senior gynecologist and fertility-focused consultant with 30+ years of experience, holding qualifications including MBBS, DGO, DNB (O&G), MRCOG (UK), and FRCOG (UK). Her expertise includes Reproductive Medicine and IVF, with specialized training at the renowned Bourn Hall Clinic, Cambridge (UK)—a globally respected pioneer in IVF history. Today, many couples don’t need “more opinions.” They need a plan. Dr Meera B’s approach is trusted because it is:- Evidence-based (no unverified claims)
- Personalized (cycle, hormones, age, history)
- Time-sensitive (does not delay next steps unnecessarily)
- Compassionate (fertility stress is real and deserves respect)
How to book an appointment with Dr Meera B
If you’re ready to stop guessing and start tracking your cycle with medical precision, you can book a consultation with Dr Meera B in just a few minutes.- Fill and submit the consultation form at https://drmeerab.com/contact/
- Call: +91 9447145101 to request scheduling an appointment
- Send a WhatsApp message using the interface on the website requesting for an appointment
About Dr Meera B
Dr. Meera. B is a highly respected gynecologist in Kollam with decades of experience in women’s health and fertility care. She completed her medical education at Govt Medical College, Trivandrum, pursued post-graduation at Govt Medical College, Kottayam, and went on to achieve prestigious UK credentials including MRCOG (2008) and FRCOG (2022). With fertility concerns rising globally and many couples silently struggling, Dr Meera B’s work bridges clinical science with compassionate care—helping patients locally in Kerala and internationally through structured evaluations, ultrasound guidance, and evidence-backed treatment pathways.Medical disclaimer
This article is for informational purposes only and does not replace medical consultation. Follicle size, ovulation timing, and treatment decisions depend on individual factors including age, hormone status, ovarian reserve, and medical history. Always consult a qualified specialist for personalized care.Frequently asked questions
In most cycles, the optimal follicle size for pregnancy is when the dominant follicle measures around 18–22 mm on scan. This range is commonly associated with a mature follicle that is ready to release an egg, giving the best chance of fertilization and implantation when timed correctly.
Dr Meera B uses follicular monitoring to help couples avoid “missed timing” cycles. Even when everything else is normal, incorrect timing can reduce pregnancy chances month after month.
Consultations with Dr Meera B are available at her place of practice including Aster PMF Hospital, Sasthamkotta.
An ovulation ultrasound is one of the most reliable ways to confirm follicle growth and estimate when ovulation is likely to occur. While apps predict ovulation based on averages and kits detect hormone changes, ultrasound directly measures the follicle and uterine lining—two factors that strongly influence real fertility outcomes.
Dr Meera B often recommends ultrasound tracking for women with irregular cycles, PCOS patterns, repeated missed fertile windows, or when couples want a clear, medically guided plan instead of guesswork.
The term 18-22 mm follicle size refers to the typical measurement of a mature dominant follicle just before ovulation. Many women ovulate naturally in this size range, which is why it is considered a practical benchmark during cycle monitoring.
That said, not every cycle follows the same pattern. Some women may ovulate at slightly smaller sizes, while others may ovulate when the follicle is larger. Dr Meera B interprets this in context—age, hormone levels, cycle length, and response to stimulation—rather than relying only on a single number.
A follicle growth chart can be helpful to understand “typical” follicle growth, especially for learning how follicles usually grow by about 1–2 mm per day after the dominant follicle is selected. However, charts are averages—not guarantees.
If your ovulation is earlier or later than expected, a chart alone may cause incorrect timing. Dr Meera B uses scan-based tracking to align timing accurately for natural conception, IUI planning, or deciding next steps.
Not always. Follicle size is a useful indicator, but it is not a perfect guarantee of egg quality. The egg inside the follicle must go through proper egg maturation, which depends on hormonal balance and healthy ovarian function.
This is why some couples feel confused when scans look “normal” but pregnancy does not happen. Dr Meera B evaluates other key factors such as ovulation confirmation, endometrial lining, thyroid/prolactin concerns, insulin resistance patterns, and semen parameters—so the plan addresses the true limiting factor.
The ideal follicle size IVF often still falls around 18–22 mm for mature eggs, but IVF is not based on one follicle. Doctors monitor a group of follicles (a cohort) and time the trigger/egg retrieval to maximize the number of mature eggs collected.
Dr Meera B’s fertility counselling helps couples understand what the scan numbers actually mean in IVF planning, so expectations remain realistic and decisions remain medically sound.
Slow or inconsistent follicle growth can happen due to stress, hormonal imbalance, thyroid/prolactin issues, PCOS-related patterns, suboptimal ovarian response, or timing problems in monitoring. It does not automatically mean infertility—but it does need evaluation.
Dr Meera B may recommend targeted blood tests, repeat tracking scans, and evidence-based ovulation induction where appropriate. The goal is to support healthy ovulation while keeping safety and ethical fertility practice at the center of care.
You can book an appointment for fertility consultation and follicular tracking with Dr Meera B by submitting the form on https://drmeerab.com/contact/ or calling +91 9447145101.
If you prefer WhatsApp, you can also send a message using the WhatsApp interface available on the website requesting an appointment. Dr Meera’s team will schedule the appointment and keep you posted.
If you have been trying for several months, timely specialist guidance can prevent further loss of cycles due to avoidable timing and monitoring gaps.

Comments are closed