How to cure endometriosis: Effective treatments & tips
Over 190 million women worldwide live with endometriosis, according to the World Health Organization—a condition that affects physical health, emotional well-being, and daily functioning. Many search online for “how to cure endometriosis,” hoping for a permanent solution. While modern medicine has not yet discovered a definitive cure, there are highly effective, scientifically proven treatments that can dramatically reduce symptoms, improve fertility, and restore quality of life. At the forefront of these advanced care options in Kerala is Dr Meera B, a globally trained gynecologist with more than three decades of clinical expertise.
This article offers clear, direct, and medically accurate guidance—answering the most pressing questions women ask and guiding you toward the right treatment pathways under Dr Meera B’s expert care at her place of practice, including Aster PMF Hospital, Sasthamkotta.
What is the most effective approach for managing endometriosis?
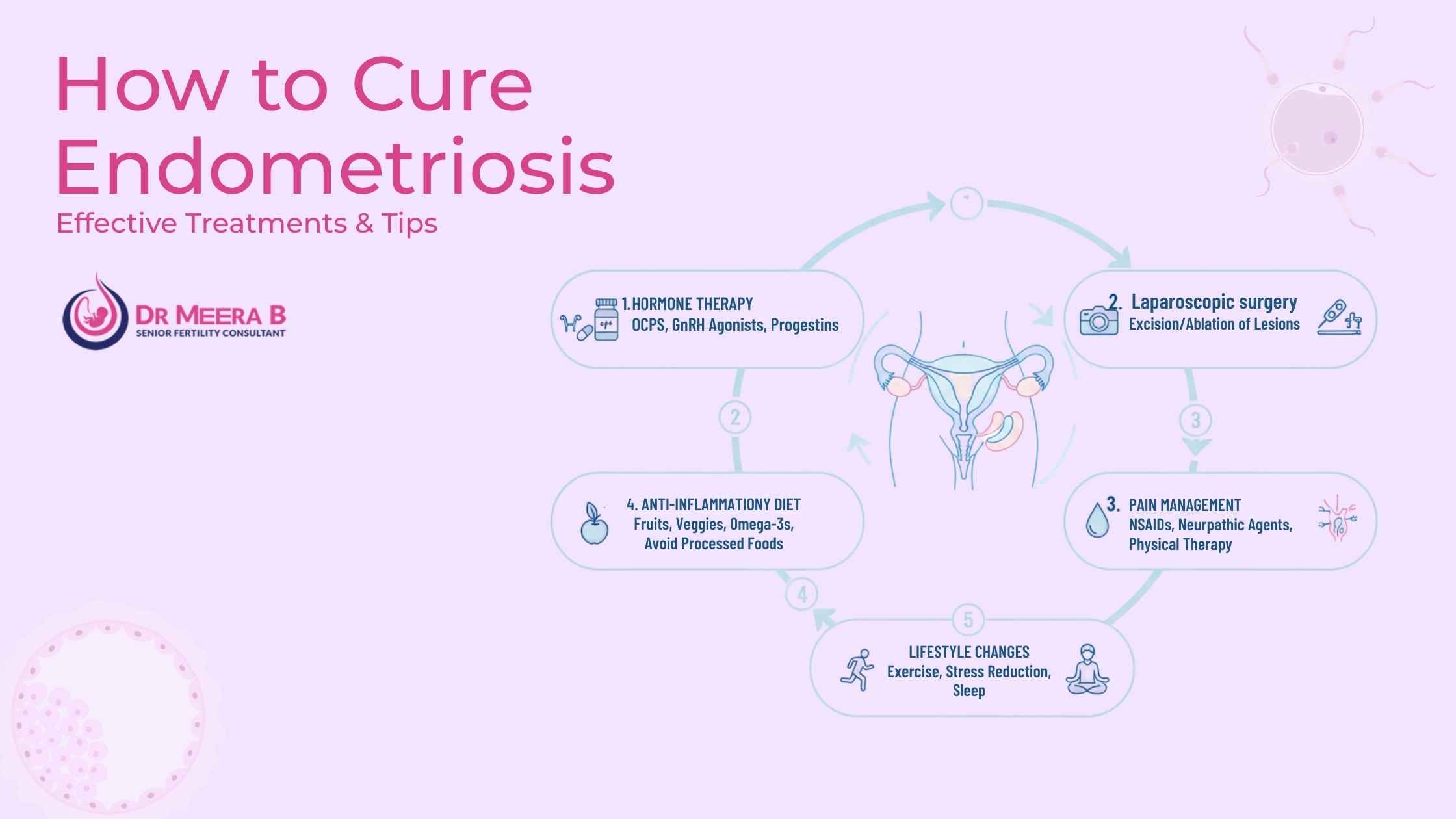
The most effective way to manage endometriosis is through a combination of medical therapy, lifestyle adjustments, and minimally invasive surgical procedures when required. Early diagnosis and tailored treatment plans significantly reduce pain and prevent progression. This is why consulting an experienced specialist like Dr Meera B is crucial to achieving long-term relief.
Endometriosis requires a personalised, multilayered approach. Throughout this article, you will find evidence-based steps, practical tips, and detailed medical insights that ensure you make informed decisions about your reproductive health.
Understanding why “cure” is a misleading term
Although people frequently search for how to cure endometriosis, the medical community clarifies that the condition currently has no permanent cure. However, symptoms can be significantly controlled or eliminated through proven treatments. Pain relief, hormonal balance, and restored fertility are highly achievable outcomes—especially with an expert handling your case.
This is where Dr Meera B’s exceptional credentials bring reassurance. With MBBS, DGO, DNB (O&G), MRCOG (UK), and FRCOG (UK), and advanced training at the world-renowned Bourn Hall Clinic, Cambridge, she is exceptionally positioned to guide patients through effective endometriosis management.
How to treat endometriosis naturally: Safe and doctor-approved methods
If you are seeking how to treat endometriosis naturally, it is important to rely only on methods that have scientific backing. Natural approaches do not replace medical treatment but can work alongside it to reduce inflammation, pain, and flare-ups.
- Anti-inflammatory diet: Foods like leafy greens, berries, nuts, and omega-3 fish can help reduce inflammatory responses.
- Regular physical activity: Gentle exercise reduces estrogen dominance and improves circulation.
- Stress-management practices: Mindfulness, stretching, and deep breathing help regulate hormonal fluctuations.
- Sleep hygiene: Consistent sleep supports immune function and hormonal regulation.
These supportive methods serve as complementary strategies—never alternatives to professional medical attention.
Is alternative healing endometriosis effective?
Many women explore alternative healing endometriosis options, but only some holistic approaches have measurable benefits. Techniques like acupuncture and pelvic physiotherapy are backed by studies showing improvements in chronic pelvic pain. However, alternative healing alone cannot remove lesions or halt disease progression. Dr Meera B incorporates these supportive therapies into a structured, evidence-based treatment plan when beneficial.
How to prevent endometriosis pain: Practical and proven strategies
The most reliable approach to how to prevent endometriosis pain is early medical intervention combined with lifestyle management. Below are doctor-approved steps that help reduce flare-ups:
- Use hormonal therapy (as prescribed) to slow lesion growth.
- Maintain anti-inflammatory dietary habits.
- Engage in regular low-impact exercise.
- Track menstrual cycles to anticipate triggers.
- Address underlying conditions like PCOS, which can worsen symptoms.
These steps do not stop endometriosis entirely but significantly reduce painful episodes.
How to relieve endometriosis cramps quickly and safely
The search for how to relieve endometriosis cramps often reveals a mix of reliable and unreliable advice. Based on clinical evidence, these methods offer consistent relief:
- NSAIDs: Anti-inflammatory medications remain the fastest method for reducing cramps.
- Heat application: Heat pads and warm showers relax pelvic muscles and improve blood flow.
- Pelvic physiotherapy: Helps realign pelvic floor tension contributing to severe cramps.
- Hormonal treatment: Reduces intensity and frequency of cramping episodes.
When cramps begin affecting daily functioning, consulting a specialist like Dr Meera B becomes essential.
When is laparoscopy needed for advanced endometriosis?
One of the most effective medical interventions is the laparoscopy procedure endometriosis, especially when symptoms persist despite medication. Laparoscopy is a minimally invasive surgery that allows direct removal of endometriotic lesions, improving pain and fertility outcomes.
Women often worry about laparoscopy endometriosis pain, but the procedure is well-tolerated and performed under anesthesia. Recovery is typically rapid, and most patients return to routine activities within a week. At her place of practice, including Aster PMF Hospital, Sasthamkotta, Dr Meera B ensures that laparoscopic intervention is recommended only when absolutely necessary and performed using the highest clinical standards.
Why choose Dr Meera B for endometriosis care?
Endometriosis requires experience, precision, and global-standard training. Dr Meera B embodies these qualities with over 30 years of dedicated gynecological practice. Her expertise in reproductive medicine, infertility solutions, and minimally invasive surgery allows her to create tailored treatment plans that restore hope and confidence.
If untreated, endometriosis can affect fertility, cause chronic pain, and reduce the quality of life. Missing the right treatment could delay years of relief—and this is why consulting Dr Meera B at the earliest sign of symptoms becomes a life-changing decision.
How to seek treatment and begin your recovery journey
Booking an appointment with Dr Meera B is simple and accessible:
- Fill in the consultation form: https://drmeerab.com/contact/
- Call: +91 9447145101
- Send a WhatsApp message through the website
Her team will guide you through scheduling and ensure a comfortable experience at her place of practice. With compassionate care, world-class training, and unwavering dedication, Dr Meera B stands as a pillar of support for women seeking freedom from endometriosis pain.
About Dr Meera B
Dr Meera B is a distinguished Obstetrician and Gynecologist, MBBS, DGO, DNB (O&G), MRCOG (UK), FRCOG (UK). She offers advanced reproductive medicine and endometriosis care across Kerala, including at Aster PMF Hospital, Sasthamkotta. Trained at the historic Bourn Hall Clinic in Cambridge—the birthplace of the world’s first IVF baby—she combines global expertise with compassionate patient care.
Frequently Asked Questions on Endometriosis Treatment with Dr. Meera B
Many women search online for how to cure endometriosis, hoping for a once-and-for-all solution. Medically, we currently do not have a guaranteed permanent cure for everyone, because endometriosis is a chronic and often hormone-dependent condition. However, with the right expert care, symptoms can often be brought under excellent control, flares can be reduced, and quality of life can dramatically improve.
In her practice, Dr. Meera B focuses on a personalised, layered approach:
- Accurate diagnosis using clinical assessment and appropriate imaging.
- Evidence-based medicines to reduce pain, bleeding, and inflammation when needed.
- Carefully planned minimally invasive surgery in selected cases.
- Support for lifestyle, nutrition, and mind–body health to reduce triggers.
For some women, this comprehensive plan leads to long periods of minimal or no symptoms. While we avoid using the word “cure” loosely, the goal with Dr. Meera’s approach is to help you feel in control of your body again and to support your fertility and long-term health as much as possible.
Dr. Meera B designs a customised treatment plan based on your age, severity of disease, pain pattern, fertility goals, and responses to any past treatments. The options may include:
- Hormonal therapies (such as certain pills, injections, or intrauterine devices) to reduce the activity of endometriosis lesions.
- Non-hormonal pain relief medicines and anti-inflammatory strategies.
- Pelvic physiotherapy and posture correction to ease muscle tension and pelvic floor dysfunction.
- Dietary guidance to minimise bloating, inflammation, and energy crashes.
- Stress-management and sleep support, which often influence flare-ups.
In women with severe pain, deep infiltrating disease, or cysts that are affecting fertility, a laparoscopy procedure endometriosis may be advised. In this minimally invasive surgery, endometriosis deposits and adhesions are carefully removed or destroyed using tiny instruments through small cuts in the abdomen. When done by an experienced specialist, laparoscopy can significantly reduce laparoscopy endometriosis pain in the long term and improve quality of life, though ongoing follow-up is still important.
Many patients ask how to treat endometriosis naturally because they want to feel active in their own healing process. Natural and lifestyle-based options can be very helpful when combined with appropriate medical care recommended by your gynecologist.
Under Dr. Meera B’s guidance, safe, evidence-informed elements of alternative healing endometriosis may be used as supportive tools, not as replacements for essential treatment. These may include:
- Anti-inflammatory nutrition patterns (more whole foods, omega-3 rich choices, and fibre; less ultra-processed food).
- Gentle movement like yoga, walking, and stretching, adjusted to your pain levels.
- Breathing exercises, meditation, and relaxation techniques to regulate the nervous system and pain perception.
- Heat therapy (hot water bottle or warm compress) applied safely to the lower abdomen or back.
Dr. Meera reviews your existing supplements and alternative therapies to ensure they do not interfere with prescribed medicines, and she discourages any unproven “miracle cures” or extreme diets that might harm your health. The aim is a balanced plan that respects your preferences while keeping you medically safe.
A common concern is how to prevent endometriosis pain from taking over everyday life. While pain may not be fully avoidable, especially during certain phases of your cycle, it can often be reduced in frequency and intensity with the right plan.
Dr. Meera B usually focuses on:
- Regulating hormones with the right treatment so lesions are less active.
- Identifying and addressing triggers like severe stress, poor sleep, or specific food patterns.
- Encouraging gentle, regular physical activity to keep blood flow and mood stable.
- Teaching pacing strategies so you do not swing between overexertion and complete rest.
She also helps you create a personalised flare-up plan: what to do when pain starts, whom to contact, which medicines you can safely take, and when it is important to seek urgent help. This sense of preparedness itself can reduce anxiety and perceived pain.
Intense period pain is one of the most distressing symptoms, and patients often ask how to relieve endometriosis cramps, especially when usual home remedies are no longer enough.
With Dr. Meera B, relief usually comes from combining several approaches rather than relying on a single method:
- Prescribed pain-relief medicines taken at the right time in your cycle (often just before pain peaks).
- Hormone-based treatments that reduce the source of pain, not just the sensation.
- Heat packs to the lower abdomen or back for short periods.
- Specific stretches, pelvic physiotherapy, and relaxation techniques to ease muscle spasm.
- Tracking your cycle and pain diary so the pattern can guide treatment adjustments.
If cramps remain severe in spite of a good medical and lifestyle plan, further evaluation is done to check for deep lesions, adhesions, or other causes that might benefit from surgical assessment.
Laparoscopy is a key tool both for diagnosing and treating endometriosis in selected cases. The laparoscopy procedure endometriosis involves inserting a tiny camera through a small cut near the navel and using fine instruments to remove or destroy visible endometriosis deposits and adhesions.
Dr. Meera B may suggest laparoscopy if you have:
- Severe or persistent pain that is not responding to medicines and lifestyle changes.
- Endometriotic cysts (endometriomas) on the ovaries that are large or symptomatic.
- Fertility concerns where endometriosis is suspected to interfere with conception.
After surgery, many women experience marked reduction in laparoscopy endometriosis pain, better mobility, and improved chances of pregnancy (depending on other factors). Recovery usually takes a few days to a couple of weeks, and Dr. Meera will discuss realistic expectations and the need for continued medical or lifestyle management to help reduce the chance of recurrence.
Endometriosis is a long-term condition, so ongoing support matters just as much as the initial treatment choice. With Dr. Meera B, care does not end after a prescription or surgery. She focuses on building a long-term relationship where you feel heard, informed, and supported.
Her follow-up care may include:
- Regular reviews to assess pain, bleeding, energy, mental health, and fertility plans.
- Adjusting medicines as your life stage changes (for example, planning pregnancy or approaching perimenopause).
- Encouraging sustainable lifestyle practices instead of extreme or short-lived changes.
- Coordinating with other professionals such as physiotherapists, nutrition experts, or mental health counsellors where needed.
The idea is to give you a personalised roadmap and a trusted specialist to walk the journey with you, rather than facing endometriosis alone or feeling confused by conflicting information online.

Comments are closed